The term diabetes mellitus describes diseases of abnormal carbohydrate metabolism that are characterized by hyperglycemia. It is associated with a relative or absolute impairment in insulin secretion, along with varying degrees of peripheral resistance to the action of insulin.
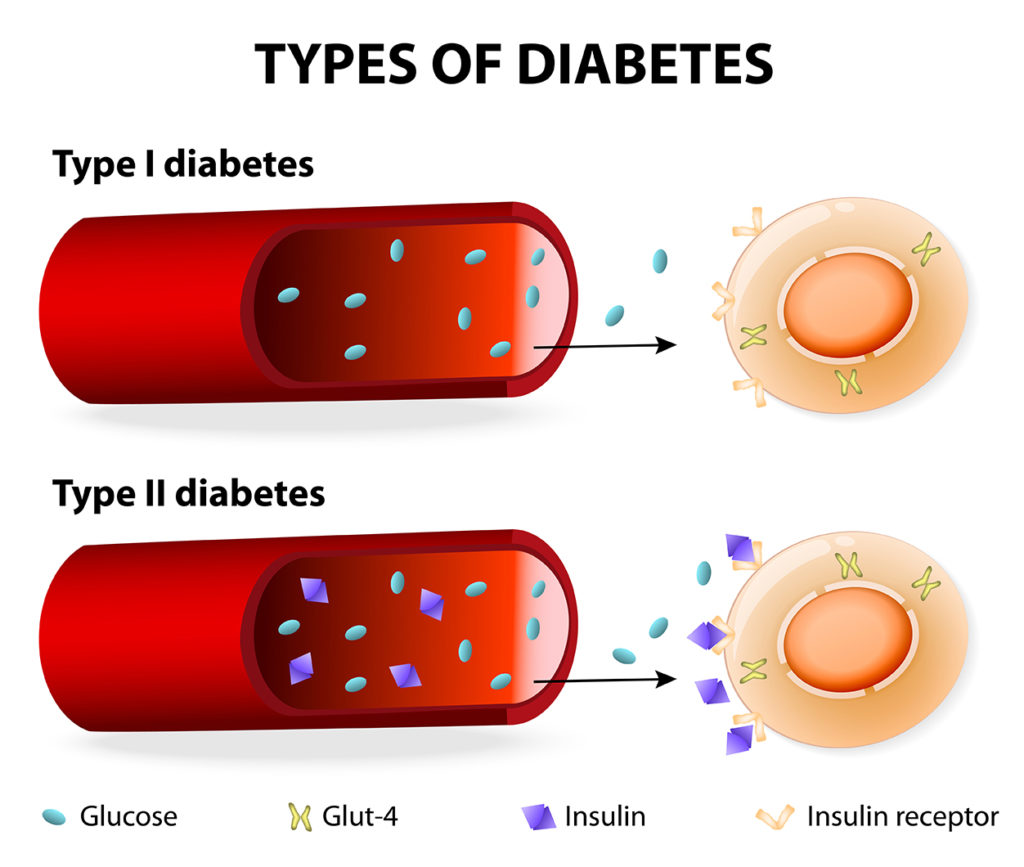
Type 1 diabetes – Type 1 diabetes is characterized by autoimmune destruction of the pancreatic beta cells, leading to absolute insulin deficiency. Type 1 diabetes accounts for approximately 5 to 10 percent of diabetes in adults. Type 1 diabetes typically have a longer estimated period prior to diagnosis and are likely to have more protracted symptoms of hyperglycemia (polyuria, polydipsia, fatigue) than children.
Diabetic ketoacidosis may be the initial presentation in approximately 25 percent of adults with newly diagnosed type 1 diabetes. Compared with children, the loss of insulin secretory capacity usually is less pronounced in adults with type 1 diabetes, and therefore, adults with type 1 diabetes typically have a longer symptomatic period (polyuria, polydipsia, weight loss, fatigue) prior to diagnosis than children.
Type 2 diabetes – Type 2 diabetes is by far the most common type of diabetes in adults (>90 percent) and is characterized by hyperglycemia usually due to progressive loss of insulin secretion from the beta cell superimposed on a background of insulin resistance, resulting in relative insulin deficiency.
The majority of patients are asymptomatic at presentation, with hyperglycemia noted on routine laboratory evaluation. The classic symptoms of hyperglycemia (including polyuria, polydipsia, nocturia, blurred vision, and weight loss).
It is a common disorder whose prevalence rises markedly with increasing degrees of obesity. Insulin resistance and insulin deficiency can arise through genetic or environmental influences, making it difficult to determine the exact cause in an individual patient.
It is occasionally difficult to distinguish between type 1 and atypical presentations of type 2 diabetes. Patients with type 1 diabetes have an absolute requirement for insulin therapy. However, many patients with type 2 diabetes lose beta cell function over time and require insulin for glucose control. Thus, need for insulin per se does not distinguish between type 1 and type 2 diabetes. While it is known that diabetic ketoacidosis (DKA) can occur in the presence of complete insulin deficiency and it is not a typical feature of type 2 diabetes, some patients with type 2 diabetes develop DKA under certain circumstances (usually severe infection or other illness).